The heart never takes a break. The heart is a strong muscle that never stops exercising, not for a minute. Every minute it needs blood, nourishment and oxygen. At Amarillo Heart Institute, we understand the importance of keeping your heart healthy and functioning at its best. We believe that a healthy heart is the foundation of a healthy life, and our goal is to provide you with all you need to achieve optimal heart health, a happier heart.
Pre-Excitation syndromes
Excitation syndromes refer to a group of cardiac disorders that result from abnormal electrical activity in the heart’s conduction system. These disorders can cause a range of symptoms, including palpitations, dizziness, fainting, and sudden cardiac death.
Wolff-Parkinson-White (WPW) Syndrome
WPW syndrome is the most common excitation syndrome. It is characterized by an abnormal electrical pathway, known as the accessory pathway, that connects the atria and ventricles. This accessory pathway can cause rapid heart rates and potentially life-threatening arrhythmias, such as atrial fibrillation (AF) and ventricular fibrillation (VF). Symptoms may include palpitations, dizziness, fainting, and chest pain. Treatment options for WPW syndrome include medication to control heart rate and rhythm, catheter ablation to destroy the accessory pathway, and surgery in rare cases.
Lown-Ganong-Levine (LGL) Syndrome
LGL syndrome is caused by an additional pathway that bypasses the atrioventricular (AV) node, which is the normal electrical connection between the atria and ventricles. Like WPW syndrome, LGL syndrome can cause rapid heart rates and arrhythmias. Symptoms may include palpitations, shortness of breath, and fainting. Treatment options for LGL syndrome are similar to those for WPW syndrome and may include medication and catheter ablation.
Mahaim Syndrome
Mahaim syndrome is caused by an accessory pathway in the right side of the heart. This pathway can cause rapid heart rates and arrhythmias, similar to WPW and LGL syndromes. However, Mahaim syndrome is less common than those two disorders. Symptoms may include palpitations, dizziness, and shortness of breath. Treatment options for Mahaim syndrome may include medication and catheter ablation.
Jervell and Lange-Nielsen Syndrome
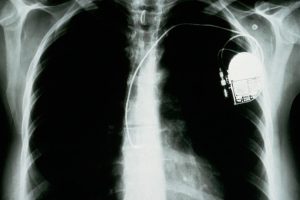
Jervell and Lange-Nielsen syndrome is a rare genetic disorder that affects the heart’s electrical activity. It is characterized by a prolonged QT interval on an electrocardiogram (ECG), which can increase the risk of a life-threatening arrhythmia known as torsades de pointes. Other symptoms may include fainting and seizures. Treatment options for Jervell and Lange-Nielsen syndrome may include medication and implantation of an implantable cardioverter defibrillator (ICD).
Brugada Syndrome
Brugada syndrome is another rare genetic disorder that affects the heart’s electrical activity. It is characterized by a distinctive pattern on an ECG known as a “coved” ST-segment elevation. This pattern can increase the risk of a potentially fatal arrhythmia called ventricular fibrillation. Symptoms may include palpitations, fainting, and sudden cardiac death. Treatment options for Brugada syndrome may include medication and implantation of an ICD.
It’s important to note that excitation syndromes can sometimes overlap or coexist with other cardiac conditions, such as coronary artery disease, hypertension, or structural heart disease. This can complicate diagnosis and treatment, and may require a multidisciplinary approach involving cardiologists, electrophysiologists, and other specialists.
How to diagnose Pre-excitation syndromes
The diagnosis of excitation syndromes typically involves a combination of medical history, physical examination, and various tests. Here are some of the most common diagnostic tests used to identify these syndromes:
Electrocardiogram (ECG): An ECG is a simple, non-invasive test that records the electrical activity of the heart. During an ECG, small electrodes are attached to the skin on the chest, arms, and legs. The test takes just a few minutes to complete and can help identify characteristic patterns of abnormal electrical activity that are associated with excitation syndromes, such as Wolff-Parkinson-White (WPW) syndrome, Lown-Ganong-Levine (LGL) syndrome, and Brugada syndrome.
Holter monitor: A Holter monitor is a portable device that records the heart’s electrical activity over a 24- or 48-hour period. The monitor is worn on the chest and connected to small electrodes that are attached to the skin. The test can help identify arrhythmias that may not be detected during a routine ECG.
Event monitor: An event monitor is similar to a Holter monitor, but it is worn for longer periods of time (up to 30 days) and only records the heart’s electrical activity when symptoms occur. The monitor can be activated by the patient when symptoms such as palpitations or dizziness are experienced, allowing for more targeted monitoring.
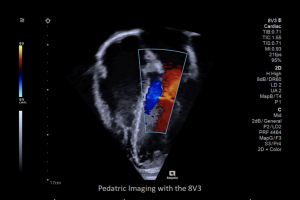
Echocardiogram: An echocardiogram is a non-invasive test that uses sound waves to create images of the heart. The test can help assess the structure and function of the heart and can be useful in identifying underlying cardiac conditions that may be associated with excitation syndromes.
Electrophysiology study (EPS): An EPS is an invasive test that is performed in a hospital setting. During the test, a small catheter is inserted through a vein in the groin and threaded up to the heart. The catheter is used to measure the heart’s electrical activity and can help identify the specific location of abnormal pathways or electrical signals that may be causing arrhythmias.
Genetic testing: In cases where a genetic disorder such as Jervell and Lange-Nielsen syndrome or Brugada syndrome is suspected, genetic testing may be performed to identify specific mutations that are associated with these conditions.
Overall, the diagnostic approach to excitation syndromes will depend on the specific symptoms and clinical history of the patient. A comprehensive evaluation by a cardiologist or electrophysiologist may be necessary to accurately diagnose and manage these conditions.
pre excitation syndromes treatment
The treatment for excitation syndromes depends on the specific type of syndrome and the severity of the symptoms. In general, treatment options may include:
Medications: Certain medications, such as beta-blockers, calcium channel blockers, and anti-arrhythmic drugs, may be used to help regulate the heart rate and prevent arrhythmias.
Radiofrequency ablation: Radiofrequency ablation is a minimally invasive procedure that uses heat to destroy the abnormal electrical pathways that are causing arrhythmias. This procedure may be used to treat conditions such as Wolff-Parkinson-White (WPW) syndrome and atrioventricular nodal reentry tachycardia (AVNRT).
Implantable cardioverter-defibrillator (ICD): An ICD is a small device that is implanted under the skin of the chest and connected to the heart with wires. The device can detect and correct life-threatening arrhythmias by delivering a shock to the heart when needed.
Pacemaker: A pacemaker is a small device that is implanted under the skin of the chest and connected to the heart with wires. The device can help regulate the heart rate by sending electrical impulses to the heart when it beats too slowly.
Lifestyle modifications: In some cases, lifestyle modifications such as reducing caffeine intake, avoiding alcohol, and quitting smoking may be recommended to help reduce the risk of arrhythmias.
Surgery: In rare cases, surgery may be necessary to correct underlying structural abnormalities in the heart that are causing arrhythmias.
It’s important to note that treatment for excitation syndromes is individualized and based on the specific needs of each patient. Treatment decisions should be made in consultation with a cardiologist or electrophysiologist who can help determine the most appropriate treatment plan.