The heart never takes a break. The heart is a strong muscle that never stops exercising, not for a minute. Every minute it needs blood, nourishment and oxygen. At Amarillo Heart Institute, we understand the importance of keeping your heart healthy and functioning at its best. We believe that a healthy heart is the foundation of a healthy life, and our goal is to provide you with all you need to achieve optimal heart health, a happier heart.
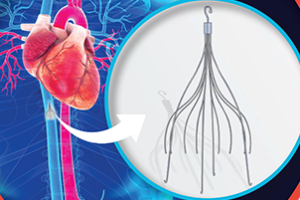
Left Atrial Appendage closure (Watchman)
Left atrial appendage closure (LAAC), also known as Watchman procedure, is a minimally invasive technique used to reduce the risk of stroke in patients with atrial fibrillation (AF), a common heart rhythm disorder. The procedure involves the placement of a small device, called the Watchman device, in the left atrial appendage (LAA), a small sac in the heart where blood can pool and form clots in patients with AF.
The procedure is performed in a cardiac catheterization laboratory (cath lab) by a team of trained medical professionals, including an electrophysiologist, an interventional cardiologist, and a cardiac surgeon.
The Watchman device has been shown to be effective in reducing the risk of stroke in patients with AF. In a clinical trial, the device was found to be non-inferior to warfarin, a commonly used blood-thinning medication, in reducing the risk of stroke, systemic embolism, and cardiovascular death in patients with non-valvular AF.
The procedure typically takes about an hour to complete and patients are usually able to go home the following day. Patients are usually required to take blood-thinning medication for several weeks after the procedure to prevent blood clots from forming around the device.
Like any medical procedure, there are potential risks and complications associated with LAAC, including bleeding, infection, device migration, and the need for repeat procedures. Patients should discuss the risks and benefits of the procedure with their doctor to determine if LAAC is right for them.Like any medical procedure, there are potential risks and complications associated with LAAC, including bleeding, infection, device migration, and the need for repeat procedures. Patients should discuss the risks and benefits of the procedure with their doctor to determine if LAAC is right for them.
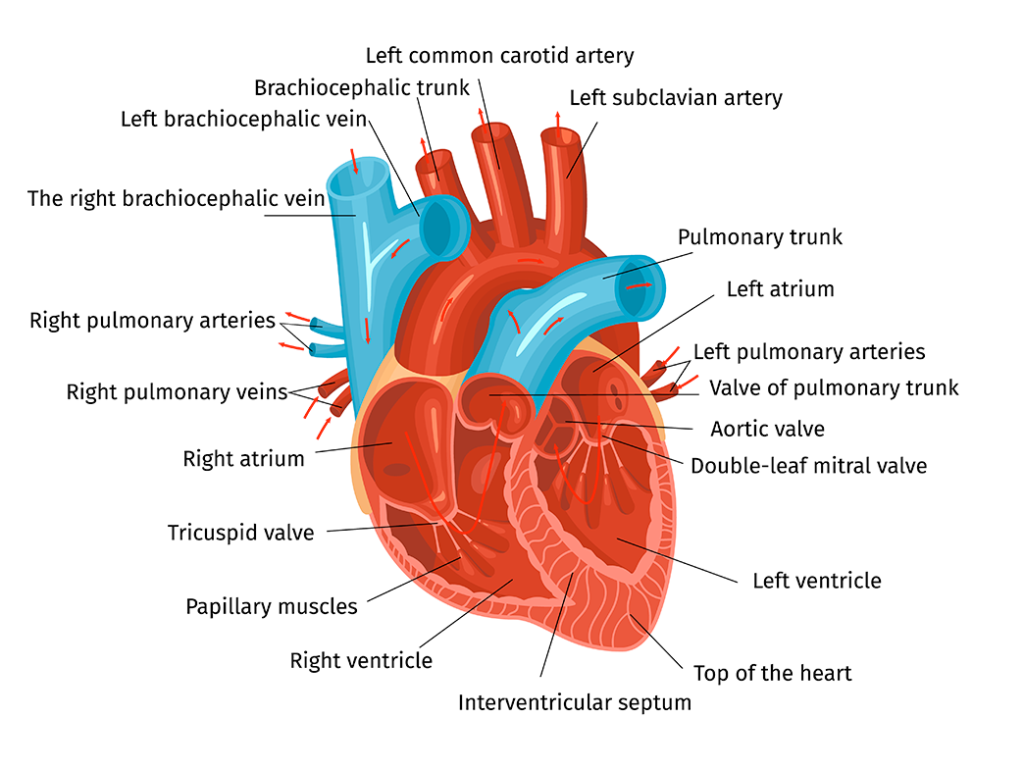
Image by macrovector on Freepik
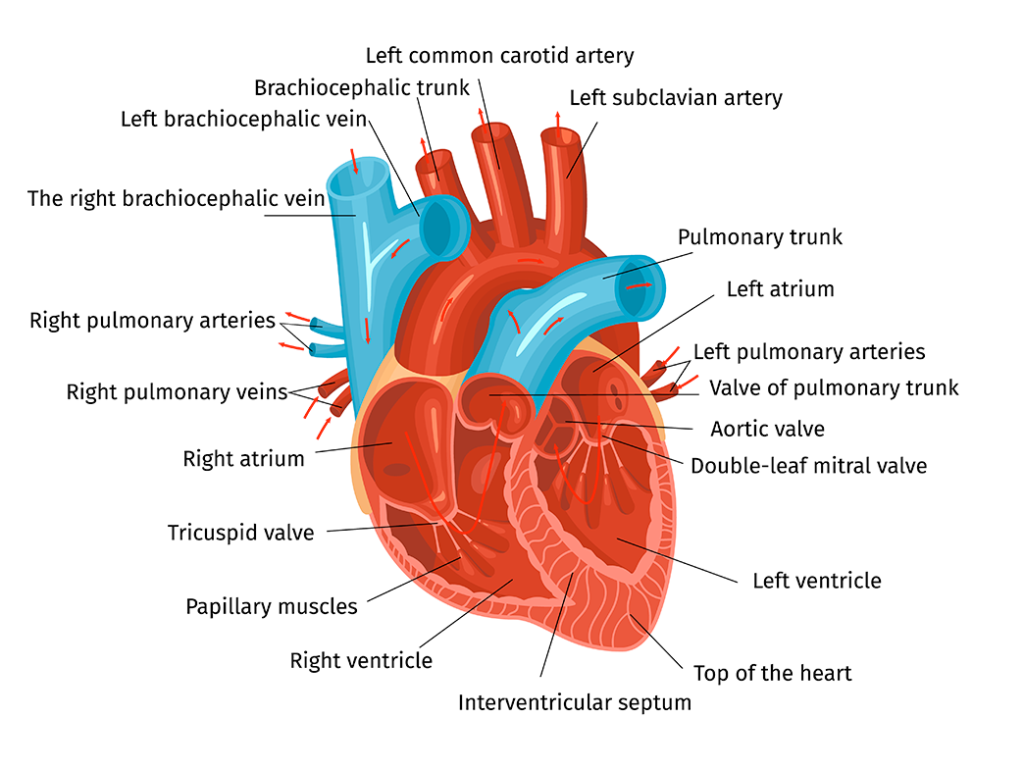
Image by macrovector on Freepik
The procedure is performed in a cardiac catheterization laboratory (cath lab) by a team of trained medical professionals, including an electrophysiologist, an interventional cardiologist, and a cardiac surgeon.
The Watchman device has been shown to be effective in reducing the risk of stroke in patients with AF. In a clinical trial, the device was found to be non-inferior to warfarin, a commonly used blood-thinning medication, in reducing the risk of stroke, systemic embolism, and cardiovascular death in patients with non-valvular AF.
The procedure typically takes about an hour to complete and patients are usually able to go home the following day. Patients are usually required to take blood-thinning medication for several weeks after the procedure to prevent blood clots from forming around the device.
Like any medical procedure, there are potential risks and complications associated with LAAC, including bleeding, infection, device migration, and the need for repeat procedures. Patients should discuss the risks and benefits of the procedure with their doctor to determine if LAAC is right for them.Like any medical procedure, there are potential risks and complications associated with LAAC, including bleeding, infection, device migration, and the need for repeat procedures. Patients should discuss the risks and benefits of the procedure with their doctor to determine if LAAC is right for them.
Before the procedure: Evaluation
The patient undergoes a thorough evaluation, including a medical history review, physical examination, electrocardiogram (ECG), and imaging tests, such as cardiac MRI, cardiac CT Scan, echocardiography, determine if they are a candidate for the procedure.
During the procedure
The patient is admitted to the cath lab and given sedation and anesthesia to make them comfortable and minimize discomfort during the procedure.
The first step of the procedure is to gain access to the femoral vein in the groin area, through which a long, thin, flexible tube called a catheter is inserted. The catheter is guided up to the heart using x-ray imaging and advanced computer technology.
Once the catheter is in place, a special imaging technique called transesophageal echocardiography (TEE) is used to visualize the left atrial appendage (LAA) and confirm its size and shape. The TEE probe is a flexible tube with an ultrasound transducer at the tip that is inserted into the esophagus to obtain high-quality images of the heart.
Once the LAA has been confirmed, a delivery sheath is inserted through the catheter and guided into the LAA. The Watchman device, which is a small, expandable device made of metal and fabric, is then inserted through the sheath and positioned in the LAA.
Once in place, the device is expanded to fit snugly inside the LAA and prevent blood from entering the appendage. Over time, the device becomes covered by tissue and forms a barrier that prevents blood clots from forming in the LAA, reducing the risk of stroke in patients with AF.
After the device is implanted, TEE is performed again to confirm that the device is properly positioned and functioning as intended.
The procedure typically takes about 1-2 hours to complete, and the patient is usually able to go home the following day. Patients are typically required to take blood-thinning medications, such as aspirin and clopidogrel, for several months after the procedure to prevent blood clots from forming around the device.