The heart never takes a break. The heart is a strong muscle that never stops exercising, not for a minute. Every minute it needs blood, nourishment and oxygen. At Amarillo Heart Institute, we understand the importance of keeping your heart healthy and functioning at its best. We believe that a healthy heart is the foundation of a healthy life, and our goal is to provide you with all you need to achieve optimal heart health, a happier heart.
Cardiomyopathies
Cardiomyopathies are a group of diseases that affect the structure and function of the heart muscle. These conditions can lead to heart failure, arrhythmias, and other complications. There are three main types of cardiomyopathy: dilated, hypertrophic, and restrictive.
Prevention of cardiomyopathy depends on the underlying causes and risk factors that can lead to the condition. Here are some general tips that may help reduce the risk of developing cardiomyopathy:

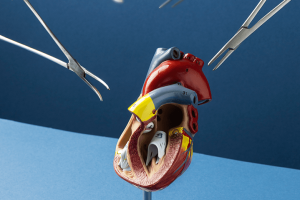
Image by Freepik
Types of Cardiomyopathies:
Dilated cardiomyopathy (DCM)
Dilated cardiomyopathy (DCM) is the most common type of cardiomyopathy. It is characterized by an enlarged heart chamber and weakened heart muscle, which make it harder for the heart to pump blood. DCM can be caused by genetic mutations, viral infections, alcohol abuse, or certain medications. Symptoms of DCM include shortness of breath, fatigue, swelling in the legs or abdomen, and arrhythmias. Treatment for DCM includes medications such as ACE inhibitors and beta-blockers, lifestyle modifications such as salt restriction and exercise, and in severe cases, heart transplant.
- Idiopathic dilated cardiomyopathy: when no specific cause can be identified
- Familial dilated cardiomyopathy: inherited genetic mutations
- Secondary dilated cardiomyopathy: caused by other factors such as viral infections, alcohol abuse, certain medications, or autoimmune diseases
Hypertrophic cardiomyopathy (HCM)
Hypertrophic cardiomyopathy (HCM) is a condition in which the heart muscle becomes abnormally thick, making it harder for the heart to pump blood. HCM is often inherited and can lead to sudden cardiac arrest in some cases. Symptoms of HCM include chest pain, shortness of breath, palpitations, and fainting. Treatment for HCM includes medications such as beta-blockers and calcium channel blockers, lifestyle modifications such as avoiding strenuous exercise, and in severe cases, surgical procedures such as septal myectomy or alcohol septal ablation.
- Obstructive HCM: when the thickened heart muscle obstructs blood flow out of the heart
- Non-obstructive HCM: when there is no obstruction of blood flow
Restrictive cardiomyopathy (RCM)
Restrictive cardiomyopathy (RCM) is a rare type of cardiomyopathy in which the heart muscle becomes stiff and rigid, making it difficult for the heart to fill with blood. RCM can be caused by a variety of factors, including certain medications, radiation therapy, and diseases such as amyloidosis. Symptoms of RCM include shortness of breath, fatigue, and swelling in the legs or abdomen. Treatment for RCM includes medications such as diuretics and heart rhythm drugs, lifestyle modifications such as salt restriction, and in some cases, heart transplant.
- Infiltrative RCM: caused by abnormal accumulation of substances such as amyloid protein, glycogen, or iron in the heart muscle
- Non-infiltrative RCM: caused by other factors such as radiation therapy, chemotherapy, or sarcoidosis
Dilated cardiomyopathy (DCM)
Dilated cardiomyopathy (DCM) is the most common type of cardiomyopathy. It is characterized by an enlarged heart chamber and weakened heart muscle, which make it harder for the heart to pump blood. DCM can be caused by genetic mutations, viral infections, alcohol abuse, or certain medications. Symptoms of DCM include shortness of breath, fatigue, swelling in the legs or abdomen, and arrhythmias. Treatment for DCM includes medications such as ACE inhibitors and beta-blockers, lifestyle modifications such as salt restriction and exercise, and in severe cases, heart transplant.
- Idiopathic dilated cardiomyopathy: when no specific cause can be identified
- Familial dilated cardiomyopathy: inherited genetic mutations
- Secondary dilated cardiomyopathy: caused by other factors such as viral infections, alcohol abuse, certain medications, or autoimmune diseases
Hypertrophic cardiomyopathy (HCM)
Hypertrophic cardiomyopathy (HCM) is a condition in which the heart muscle becomes abnormally thick, making it harder for the heart to pump blood. HCM is often inherited and can lead to sudden cardiac arrest in some cases. Symptoms of HCM include chest pain, shortness of breath, palpitations, and fainting. Treatment for HCM includes medications such as beta-blockers and calcium channel blockers, lifestyle modifications such as avoiding strenuous exercise, and in severe cases, surgical procedures such as septal myectomy or alcohol septal ablation.
- Obstructive HCM: when the thickened heart muscle obstructs blood flow out of the heart
- Non-obstructive HCM: when there is no obstruction of blood flow
Restrictive cardiomyopathy (RCM)
Restrictive cardiomyopathy (RCM) is a rare type of cardiomyopathy in which the heart muscle becomes stiff and rigid, making it difficult for the heart to fill with blood. RCM can be caused by a variety of factors, including certain medications, radiation therapy, and diseases such as amyloidosis. Symptoms of RCM include shortness of breath, fatigue, and swelling in the legs or abdomen. Treatment for RCM includes medications such as diuretics and heart rhythm drugs, lifestyle modifications such as salt restriction, and in some cases, heart transplant.
- Infiltrative RCM: caused by abnormal accumulation of substances such as amyloid protein, glycogen, or iron in the heart muscle
- Non-infiltrative RCM: caused by other factors such as radiation therapy, chemotherapy, or sarcoidosis
Overall, cardiomyopathies are a group of heart muscle diseases that can lead to heart failure, arrhythmias, and other complications. Treatment for cardiomyopathies involves a combination of medications, lifestyle modifications, and, in severe cases, surgical procedures or heart transplant. It is important for medical students to be able to recognize the different types of cardiomyopathies and their symptoms, as well as the appropriate treatment options for each type.
CAUSES OF Cardiomyopathies
The causes of cardiomyopathies can vary depending on the specific subtype. However, some common causes and risk factors for cardiomyopathies include:
- Genetic mutations: Many cardiomyopathies have a genetic component, meaning that certain genes may be passed down from parents that increase the risk of developing the condition.
- Infections: Certain infections, such as viral infections, can cause inflammation of the heart muscle and lead to cardiomyopathy.
- Alcohol and drug abuse: Long-term alcohol and drug abuse can damage the heart muscle and lead to cardiomyopathy.
- Chemotherapy drugs: Certain chemotherapy drugs used to treat cancer can cause damage to the heart muscle and lead to cardiomyopathy.
- Autoimmune disorders: Autoimmune disorders, such as lupus or rheumatoid arthritis, can cause inflammation of the heart muscle and lead to cardiomyopathy.
- Nutritional deficiencies: Certain nutritional deficiencies, such as deficiencies in thiamine or selenium, can lead to cardiomyopathy.
- Idiopathic: In some cases, the cause of cardiomyopathy may be unknown or idiopathic.
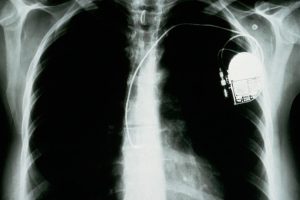
It’s important to note that some cardiomyopathies may have multiple causes or may be caused by a combination of genetic and environmental factors. Treatment for cardiomyopathy will depend on the specific subtype and underlying cause, and may include medications, lifestyle changes, and in some cases, surgery or implanted devices such as pacemakers or defibrillators.
How to diagnose Cardiomyopathies
The diagnosis of cardiomyopathy typically involves a combination of medical history, physical examination, and diagnostic tests. Here are some common methods used to diagnose cardiomyopathies:
Medical history: Your healthcare provider will ask about any symptoms you may be experiencing, as well as any personal or family history of heart disease or other related conditions.
Physical examination: Your healthcare provider will perform a physical examination to check for signs of heart problems, such as an enlarged heart or abnormal heart sounds.
Electrocardiogram (ECG): An ECG records the electrical activity of the heart and can help identify abnormal rhythms or other heart problems.
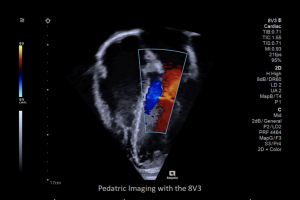
Echocardiogram: An echocardiogram uses sound waves to create images of the heart, allowing healthcare providers to see the structure and function of the heart.
Cardiac MRI: A cardiac MRI uses magnetic fields and radio waves to create detailed images of the heart, allowing healthcare providers to see the structure and function of the heart.
Blood tests: Blood tests can help identify certain markers or proteins that may be associated with cardiomyopathy or other heart conditions.
Genetic testing: Genetic testing may be recommended for individuals with a family history of cardiomyopathy or other heart conditions.
Depending on the specific type of cardiomyopathy and underlying causes, additional diagnostic tests may be necessary. Your healthcare provider will work with you to determine the most appropriate diagnostic tests based on your individual situation.
How to treat Cardiomyopathies
The treatment of cardiomyopathies depends on the specific type and underlying cause. Here are some common treatment approaches:
Medications: Medications may be prescribed to manage symptoms, improve heart function, and prevent complications. Common medications used to treat cardiomyopathy include ACE inhibitors, beta-blockers, diuretics, and anticoagulants.
Lifestyle modifications: Lifestyle modifications such as a heart-healthy diet, regular exercise, weight management, and avoiding alcohol and tobacco may be recommended to improve heart health and manage symptoms.
Implantable devices: For certain types of cardiomyopathy, such as dilated cardiomyopathy, implantable devices such as pacemakers, implantable cardioverter-defibrillators (ICDs), and cardiac resynchronization therapy (CRT) devices may be recommended to help manage heart rhythm and improve heart function.
Surgery: In some cases, surgery may be necessary to treat cardiomyopathy. Examples include septal myectomy, which involves removing part of the thickened heart muscle in hypertrophic cardiomyopathy, or heart transplant, which may be recommended in severe cases of heart failure.
Genetic counseling: For individuals with familial cardiomyopathy, genetic counseling may be recommended to help identify other family members who may be at risk and provide guidance on genetic testing and family planning.
Treatment plans for cardiomyopathy are individualized based on the specific type and underlying causes, as well as the individual’s overall health status and preferences. Your healthcare provider will work with you to develop a treatment plan that best meets your needs.
How to prevent Cardiomyopathies
Maintain a healthy lifestyle: Eating a healthy diet, staying physically active, and avoiding smoking and excessive alcohol consumption can all help reduce the risk of developing cardiomyopathy.
Manage underlying conditions: If you have conditions that increase the risk of developing cardiomyopathy, such as high blood pressure, diabetes, or high cholesterol, work with your healthcare provider to manage them effectively.
Get regular checkups: Regular visits with your healthcare provider can help identify and manage any health issues that may increase the risk of developing cardiomyopathy.
Take medications as prescribed: If you have a condition that requires medication, make sure to take them as prescribed and follow your healthcare provider’s instructions closely.
Get vaccinated: Certain infections, such as viral infections, can lead to inflammation of the heart muscle and cardiomyopathy. Getting vaccinated against these infections, such as the flu or COVID-19, can help reduce the risk.
Avoid certain medications: Some medications, such as certain chemotherapy drugs or medications that can cause damage to the heart, can increase the risk of developing cardiomyopathy. If you are taking medication, talk to your healthcare provider about any potential risks.
It’s important to note that some forms of cardiomyopathy, such as genetic cardiomyopathies, may not be preventable. If you have a family history of cardiomyopathy or other heart conditions, talk to your healthcare provider about steps you can take to manage your risk.